Imagine waking up after a full night’s sleep and still feeling utterly drained, as if you hadn’t rested at all. Now, envision that this exhaustion lingers for months or even years, impacting every facet of your life. This is the daily reality for millions of people suffering from Chronic Fatigue Syndrome (CFS). Despite being a life-altering condition, CFS is often misunderstood and misdiagnosed, leaving many sufferers feeling isolated and hopeless. But there is hope. Understanding CFS and taking the right steps can help manage its symptoms and improve your quality of life.

Table of Contents
What Is Chronic Fatigue Syndrome (CFS)?
Chronic Fatigue Syndrome, also known as Myalgic Encephalomyelitis (ME/CFS), is a complex and debilitating disorder characterized by extreme fatigue that doesn’t improve with rest. The fatigue experienced with Chronic Fatigue Syndrome is not the kind of tiredness that can be brushed off with a good night’s sleep. It is profound, persistent, and can significantly interfere with daily activities.
CFS can affect anyone, regardless of age, gender, or background. However, it is more commonly diagnosed in women, particularly those in their 40s and 50s. The exact cause of Chronic Fatigue Syndrome remains unknown, but several factors, including viral infections, immune system problems, hormonal imbalances, and psychological stress, may contribute to its development. Research is ongoing, but the complex nature of Chronic Fatigue Syndrome means that a single cause may never be identified. Instead, it is likely that a combination of factors triggers the onset of the condition.
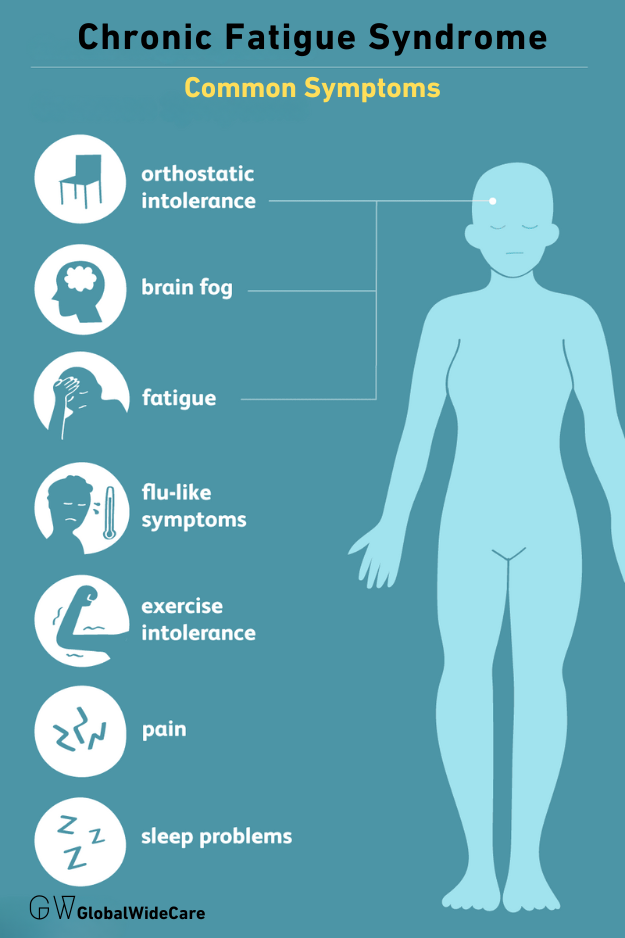
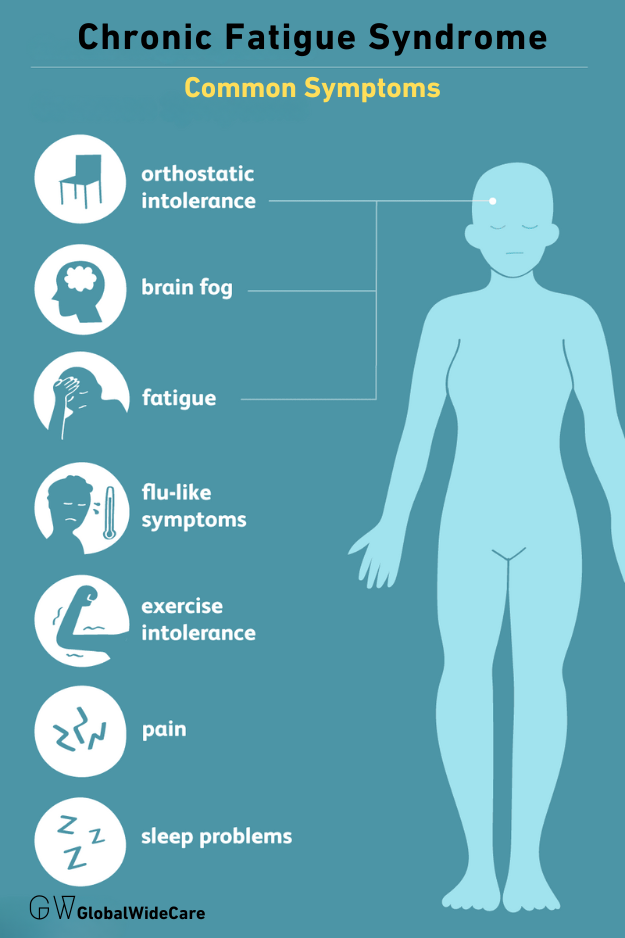
Symptoms That You Shouldn’t Ignore
CFS is much more than just fatigue. It comes with a wide range of other symptoms that can be just as debilitating, including:
- Unrefreshing sleep: Even after a long sleep, you still feel exhausted. This unrefreshing sleep is one of the hallmark symptoms of Chronic Fatigue Syndrome and can be deeply frustrating for sufferers, as rest does not provide the expected relief.
- Cognitive difficulties: Often referred to as “brain fog,” this includes problems with memory, concentration, and attention. Many people with CFS struggle to perform tasks that require mental effort, leading to difficulties at work or in school.
- Muscle and joint pain: Unexplained pain that is not due to physical exertion. This pain can range from mild discomfort to severe, debilitating pain, and it often moves around the body.
- Headaches: Frequent or severe headaches that may feel different from usual. These headaches can be persistent and may not respond to typical pain relief methods.
- Sore throat or swollen lymph nodes: Symptoms that may persist without a clear infection. These symptoms can be misleading and are often mistaken for signs of a common cold or flu, but in the context of CFS, they may be a sign of something more chronic.
- Post-exertional malaise (PEM): A worsening of symptoms following physical or mental exertion, sometimes lasting days or even weeks. PEM is one of the most challenging aspects of Chronic Fatigue Syndrome, as even minor activities can trigger a significant flare-up of symptoms, leaving sufferers bedridden.
Proven Ways to Manage CFS
While there is currently no cure for CFS, several strategies can help manage the symptoms and improve your quality of life. Here are seven proven ways to take control of your health if you’re living with Chronic Fatigue Syndrome:
1. Pacing Yourself
One of the most effective strategies for managing Chronic Fatigue Syndrome is pacing, which involves balancing activity and rest to avoid the post-exertional malaise (PEM) that many sufferers experience. Pacing is about learning to listen to your body and recognizing when you need to stop and rest before you reach the point of exhaustion.
- Energy envelope: Identify your “energy envelope,” the amount of activity you can do without triggering a flare-up, and try to stay within it. This might mean adjusting your expectations and cutting back on activities that you used to take for granted.
- Break tasks into smaller steps: Instead of pushing through a task, break it down and take frequent breaks. For example, if you need to clean your house, consider tackling one room at a time and resting in between. This approach can help prevent overexertion and reduce the risk of triggering PEM.
- Use a diary: Keeping a diary of your activities and symptoms can help you identify patterns and better manage your energy levels. This can also be a valuable tool when working with healthcare providers to develop a management plan.


2. Prioritizing Sleep
Quality sleep is crucial for everyone, but for those with CFS, it’s even more important. However, getting good sleep can be challenging due to the unrefreshing nature of sleep associated with Chronic Fatigue Syndrome. Addressing sleep issues can be one of the most effective ways to manage CFS symptoms.
- Create a bedtime routine: Stick to a consistent sleep schedule, even on weekends. Going to bed and waking up at the same time every day can help regulate your body’s internal clock and improve sleep quality.
- Optimize your sleep environment: Ensure your bedroom is cool, dark, and quiet. Invest in a comfortable mattress and pillows. Consider using blackout curtains, white noise machines, or earplugs to create a sleep-friendly environment.
- Limit screen time: The blue light emitted by phones, tablets, and computers can interfere with your ability to fall asleep. Try to avoid screens for at least an hour before bed, and instead, engage in relaxing activities like reading or taking a warm bath.
3. Diet and Nutrition
The right nutrition can have a significant impact on your energy levels and overall well-being. A balanced diet can provide the nutrients your body needs to function optimally, while certain foods may help alleviate some symptoms of CFS.
- Balanced diet: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. These foods provide essential vitamins and minerals that support overall health and energy levels.
- Stay hydrated: Dehydration can exacerbate fatigue, so drink plenty of water throughout the day. Aim for at least eight glasses of water daily, and more if you are physically active or live in a hot climate.
- Consider supplements: Some people with Chronic Fatigue Syndrome benefit from supplements like B vitamins, magnesium, and omega-3 fatty acids, but consult a healthcare provider before starting any new supplements. These nutrients can help support energy production, reduce inflammation, and improve cognitive function.
- Avoid processed foods: Processed foods are often high in sugar, unhealthy fats, and artificial additives, which can contribute to inflammation and worsen symptoms. Instead, focus on whole, unprocessed foods that nourish your body.


4. Mind-Body Therapies
Mind-body therapies, such as meditation, yoga, and deep breathing exercises, can help manage the stress and anxiety often associated with Chronic Fatigue Syndrome. These therapies can also improve mental clarity, reduce pain, and promote relaxation.
- Meditation: Regular meditation can help calm the mind and improve focus. Start with just a few minutes a day and gradually increase the duration as you become more comfortable with the practice. Meditation apps or guided meditations can be helpful if you’re new to the practice.
- Gentle yoga: Low-impact yoga can improve flexibility and reduce muscle tension. Choose a style of yoga that is gentle and restorative, focusing on slow movements and deep breathing. Avoid intense or vigorous styles that could trigger PEM.
- Deep breathing exercises: These can help reduce stress and increase oxygen flow to the body. Practice deep, diaphragmatic breathing by inhaling slowly through your nose, allowing your abdomen to expand, and then exhaling slowly through your mouth. This type of breathing can help calm the nervous system and promote relaxation.


5. Cognitive Behavioral Therapy (CBT)
CBT is a type of psychotherapy that helps individuals change negative thought patterns that can contribute to the severity of their symptoms. While CBT is not a cure for Chronic Fatigue Syndrome, it can be a valuable tool for managing the psychological aspects of the condition.
- Challenge negative thoughts: Learn to reframe thoughts that may be contributing to your feelings of helplessness. For example, instead of thinking, “I’ll never be able to do anything again,” try to focus on the things you can do and the progress you’ve made.
- Develop coping strategies: CBT can help you develop practical strategies for managing your symptoms and improving your daily functioning. This might include setting realistic goals, developing a daily routine, or learning relaxation techniques.
- Work with a therapist: A trained CBT therapist can guide you through the process and help you develop personalized strategies for managing Chronic Fatigue Syndrome. Many therapists offer online sessions, making it easier to access care from the comfort of your home.
6. Physical Therapy
Though exercise can be challenging for those with Chronic Fatigue Syndrome, gentle physical therapy tailored to your energy levels can help improve muscle strength and flexibility without triggering PEM. Working with a physical therapist who understands Chronic Fatigue Syndrome is essential to developing a safe and effective exercise plan.
- Graded Exercise Therapy (GET): Start with very low-intensity exercises and gradually increase as tolerated. GET should be approached with caution, as it can worsen symptoms if not carefully managed. Always listen to your body and stop if you feel your symptoms worsening.
- Stretching and mobility exercises: These can help maintain flexibility and reduce stiffness. Focus on gentle stretches that don’t push your body too hard. Stretching can also be incorporated into your daily routine to help prevent stiffness and improve circulation.
- Strength training: Light strength training exercises using body weight or resistance bands can help maintain muscle mass and strength. Avoid heavy weights or intense resistance, as these could trigger a flare-up of symptoms.
7. Seeking Support
Living with Chronic Fatigue Syndrome can be incredibly isolating, but you don’t have to go through it alone. Connecting with others who understand your experience can provide emotional support and practical advice.
- Support groups: Join online or in-person support groups where you can share your experiences and learn from others. Many people with Chronic Fatigue Syndrome find comfort in knowing they are not alone and can gain valuable insights from others who have navigated similar challenges.
- Counseling: Speaking with a counselor or therapist can help you cope with the emotional challenges of living with Chronic Fatigue Syndrome. Therapy can provide a safe space to explore your feelings, develop coping strategies, and address any mental health concerns that may arise.
- Communicate with loved ones: Help your family and friends understand what you’re going through. Open and honest communication can foster understanding and support, making it easier for your loved ones to offer help when needed.
Conclusion
Chronic Fatigue Syndrome is a complex and often misunderstood condition that can have a profound impact on your life. However, by taking proactive steps to manage your symptoms, you can improve your quality of life and regain a sense of control. Remember, managing Chronic Fatigue Syndrome is a journey, and what works for one person may not work for another. Be patient with yourself, and don’t hesitate to seek support from healthcare professionals and others who understand what you’re going through.
For those looking for more information on managing Chronic Fatigue Syndrome, consider exploring the following resources:
By staying informed and actively managing your health, you can take steps toward a healthier, more fulfilling life despite the challenges of Chronic Fatigue Syndrome.